Spinal Conditions
Back and neck pain are common yet can be difficult problems to deal with. Approximately 80% of adults will experience low back pain in their lifetime, and 20%-40% of the adults have had neck pain in the last month. Those aged 25 to 60 are most usually affected, but no age is completely immune
The spine is a complex structure composed of bones, muscles, ligaments, tendons, joints, discs, and nerves, all working together to provide both structural support and mobility. Although your pain may come from a specific part of your spine, often more than one part is involved.
The following is a list of the various spinal ailments afflicting adults today.
Arthritis - is a term that indicates inflammation of the joints. A joint is an articulation between bones that provides stability along with varying types and degrees of motion. Spinal arthritis is often associated with osteoarthritis and with the loss of cartilage found on the joint surfaces. The spinal joints are the facet joints, however the term “arthritis” is also sometimes used to describe degenerative or “wear and tear” changes of the discs (see “Degenerative Disc Disease” below). “Arthritis” of the spine is frequently diagnosed based on the presence of degenerative changes seen on imaging studies such as x-rays, MRI and/or CT scans. Like “degenerative disc disease” it is part of the normal aging process and is frequently seen in people without spinal symptoms
Cervical Spinal Stenosis and Myelopathy - as we age the discs
lose their ability to hold water, leading loss of disc height and bulging into the spinal canal. The bones and ligaments of the spinal joints can thicken, also narrowing the spinal canal. When
this narrowing of the spinal canal happens in the neck it is known as “Cervical Spinal Stenosis”, and when the spinal cord is
compressed enough to cause injury and loss of function this is called “Cervical Myelopathy”.
Cervical Stenosis
does not necessarily cause symptoms, however patients with cervical myelopathy often have arm and/or leg symptoms including weakness, clumsiness in the hands, (inability to button a shirt, open a
jar, etc.). Leg symptoms may include weakness, and difficulty with balance and walking. Urinary urgency can also occur
The diagnosis is
established by a focused history and examination. Findings that are suggestive of cervical stenosis and myelopathy include increased deep tendon reflexes (called hyperreflexia), loss of
balance, loss of sensation and/or position sense in the hands and/or feet, rapid foot movement triggered by moving the ankle upward (called clonus), extension of the big toe when the bottom of the foot is stroked (called Babinski’s sign), and/or contraction of the thumb and index finger
after flipping of the middle finger toward the palm (called Hoffman’s sign). X-rays do not adequately view the spinal canal and are done primarily to rule out other conditions. MRI scans are
commonly performed, and in some instances a CT scan performed with dye may add useful information.
There is
variability in the progression of cervical stenosis and myelopathy. Some patients slowly decline, some stabilize and others rapidly decline. There are a variety of surgical procedures that can
be performed depending upon each patient’s individual circumstances.
Degenerative Disc Disease – This term, also known as Disc Degeneration, can cause confusion and anxiety for patients when they are told that this is the cause of their spinal pain. These conditions sound like they are irreversible and will worsen as one grows older. This can make a patient think that their condition will become more debilitating over time. However these terms describe the normal aging process of the spinal discs, not a “disease”. While everyone experiences changes in their discs, it is usually not painful and the presence of degenerative changes seen in tests such as x-rays and MRI scans are frequently seen in people without spinal symptoms.
The vertebrae (bones) of the spinal column are separated from each other by cartilaginous cushions known as intervertebral discs. The discs provide structural support to the spine and act as shock absorbers, taking in the stress created by movement. The discs hold water, allowing them to be very elastic and absorb stress. However, age, repetitive strain, and genetics cause the discs to lose the ability to hold water leading to wear and tear of the disc.
The terms “Degenerative Disc Disease” or “Disc Degeneration” are usually based on findings from imaging studies such as x-rays or MRI scans. These terms do not always provide an accurate or useful diagnosis as these changes are commonly seen in people without symptoms. Treatment decisions are based on a combination of factors that emphasize the patient history and exam, and are not made solely on the basis of structural findings. As such, these terms do not really describe clinical conditions in a manner that leads to meaningful patient and health care provider decision making.
Discogenic Back or Neck Pain - refers to pain coming from the
disc. While there are many causes of back and neck pain, the disc is felt to be a common cause of pain. There are often clues in the patient’s history and examination that lead to this
diagnosis. Usually, in a patient with discogenic low back pain, sitting worsens the pain more than standing and walking will provide some relief. Bending forward, twisting, and lifting also generally
worsen the pain and lying down for short periods can reduce the pain. Patients with discogenic neck pain will usually experience worse symptoms with their head held in a forward position or with the
neck flexed forward or looking down. Patients with discogenic back or neck pain can also have pain in their legs or arms, but the pain is often “an ache” that appear "normal" upon physical
examination tests for nerve irritation and tension.
Imaging studies can
also be performed, such as MRI, for patients with severe or worsening symptoms. However, because disc degeneration is part of normal aging, MRI scans, x-rays and other imaging tests often show
“abnormalities” in those with no symptoms as well. Therefore, it is difficult to truly know that any disc is truly causing the symptoms based on the imaging tests alone, even if the disc appears
“abnormal” on an imaging test. A discogram, an injection of dye into the disc, is reserved for those rare cases where surgery is being considered for persistent spinal pain thought to coming from the
disc. If the injection requires less physical resistance than normal to perform, the discogram reproduces the patients’ symptoms, and there are structural findings of dye leakage on imaging tests,
then it is considered a positive, or concordant, discogram.
Treatment
for discogenic back or neck pain at Lane Chiropractic and Rehabilitation usually emphasizes patient education regarding body positioning, posture and exercise. Anti-inflammatory medications can
be helpful, especially for a recent acute episode. Surgery is only recommended for well selected patients with severe symptoms and activity intolerance, who have not improved with high quality
non surgical treatment. Historically fusion surgeries have been performed for these well selected patients.
Disc Herniation - A disc is composed of two parts: an outer rim of fibrous (tough) tissue called the annulus surrounding an inner loose visco-elastic fluid called the nucleus. When there is a break in the outer rim, the inner material can leak out of the disc space and enter the spinal canal where the disc material can compress nerve roots or the spinal cord and cause pain.
Compression on the nerves in the lower back can cause sciatica or shooting pain down one or both legs, typically in a distribution specific for each nerve root. In addition to mechanical compression, the disc material also contains chemicals that cause inflammation of the nerve root. Back pain can occur but often the predominant symptoms are in the leg. Furthermore, other symptoms such as weakness or numbness can occur. A similar situation can occur in the neck where there is pain, numbness or weakness in one or both arms. Less frequently there can be spinal cord compression in the neck causing leg symptoms (see Cervical Spinal Stenosis and Myelopathy below).
The pain associated with a lumbar disc herniation usually improves with lying down and worsens with prolonged sitting, bending forward and/or lifting. Standing or walking can relieve symptoms in some cases. Very rarely, loss of control of the bowel or bladder which may be accompanied by numbness in the groin or buttock area, may occur. This type of situation requires urgent surgical decompression of the nerves under pressure. Severe or progressive loss of strength in one or both legs, (or in the arms when there is a symptomatic disc herniation in the neck), is uncommon but can also require urgent surgical treatment.
The vast majority of patients with symptoms from a disc herniation improve without surgery. Non-surgical treatment is the primary focus for our disc herniation patients and focuses initially on specific exercises, manual and other physical treatment methods based on the effect of movements or activities on each patient’s pain. This is based on the work of Robin McKenzie a New Zealand physical therapist, “the McKenzie approach”, as well as others. Endurance and strengthening exercises are introduced as patients improve. There are a subgroup of patients who benefit from traction, however some of the claims about the efficacy of “decompression therapy” which utilizes traction, are not supported by objective high quality evidence.
Anti-inflammatory medication can be helpful due to the inflammatory chemicals in the disc. In some
instances a spinal injection of cortisone (a more powerful anti-inflammatory agent), known as an epidural steroid injection (ESI), can significantly reduce a patient’s symptoms, allow for progression
of physical activity and exercise, and speed recovery. For patients who fail to respond to non-surgical treatment or have more severe symptoms, there is growing evidence that lumbar microdiscectomy
results in greater improvement than continued non-surgical treatment. Lumbar microdiscectomy typically is performed in an outpatient setting and has a high success rate with minimal risk of
complication. At Lane Chiropractic and Rehabilitation, we do not hesitate to refer these patients to MD's for medication and/or surgical intervention.
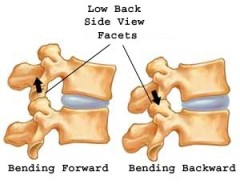
Facet Syndrome - is the term used to describe back or neck pain that comes from the facet joints of the spine. The facets are small joints that are found on both sides in the back part of the spine. A small capsule surrounds each facet joint holding the bones together and providing a nourishing lubricant for the joint. The facets help control movement in the spine.
Facet syndrome is usually diagnosed through a focused history and examination. The pain is usually felt over a fairly small area on the side of the spine, and can be on one or both sides. Sometimes there is an “ache” type of pain that is felt into the leg or arm, but it usually doesn’t follow a specific nerve path. Patients with lumbar facet syndrome typically have pain that is worse with standing and bending backward with twisting. Cervical facet pain is usually increased with looking up while turning the head/neck. Degenerative changes of the facets are commonly seen on imaging tests of people without pain. A facet joint can hurt without evidence of structural damage or changes on imaging studies such as X-ray, MRI scan or CT scans.
The majority of the time facet joint syndrome is treated with “hands-on” or manual approaches such as joint mobilization and/or
manipulation (especially for patients with restricted and painful spinal motion), stretching and strengthening exercises, and education on good spine posture. Anti-inflammatory medications can be
helpful. Facet joint injections with cortisone can also help. Anesthetic procedures that block the pain messages from the nerves to the facet joints can help confirm the diagnosis, and if there is
good short term relief with this type of injection, a procedure called Radiofrequency Rhizotomy can be performed. Surgery is rarely required.
Lumbar Spinal Stenosis - Spinal stenosis refers to narrowing of the spinal canal which can cause pressure on the spinal nerves or cord. This condition is mostly seen in patients over the age of 50. There are several causes, and two main types are described below.
The congenital form of spinal stenosis is seen in individuals who are born with a narrow spinal canal. In these individuals, minimal changes in the structure of the spine can cause severe spinal stenosis. The more common acquired form of stenosis is caused by progressive changes in different spinal elements (such as the discs, joints, ligaments, etc.) As people age, all these different elements bulge or thicken, narrowing the spinal canal.
Patients with lumbar spinal stenosis complain mainly of leg pain which worsens with walking. The medical term for this is
neurogenic claudication. Poor circulation can cause similar complaints. Back pain is also commonly seen with this problem. The leg pain is often improved with sitting or bending over. Rarely, bowel
or bladder symptoms or progressive weakness can occur; these symptoms are very severe and necessitate immediate surgery.
Many people have evidence of lumbar spinal stenosis on imaging studies, without any pain or other symptoms. Like other
spinal conditions the imaging findings should always be considered in relation to each individual patient’s history and examination findings.
Non-surgical treatment for symptomatic lumbar spinal stenosis at usually involves stretching, and endurance exercises, typically emphasizing abdominal muscular control and endurance. Manual and other physical procedures utilizing specialized treatment tables can provide relief and help patients progress with exercise. Medications can include those known as neuropathic pain medications, and epidural steroid injections can be provide relief of leg symptoms. Surgery typically involves a procedure to create more room for the nerves.
Mechanical Back or Neck Pain - mechanical back or neck pain are broad terms that encompass the most common types of spinal pain. “Mechanical” means the source of the pain is coming from one or more spinal structures - the spinal joints, discs, muscles, or other soft tissues. Mechanical pain is often increased with certain movements and positions and worse with other movements and positions.
The diagnosis of mechanical back or neck pain is established with a careful patient history and a focused physical and mechanical
examination. There is growing evidence that not all patients have the same “mechanical” cause of their spinal pain, and that individualized treatment based on each individual patient’s “mechanical”
factors results in better treatment outcomes. There are a variety of different approaches to treatment depending on the cause of the pain.
Myofascial Back or Neck Pain - means the muscles are the cause
of the pain. This can be a single muscle or a group of muscles. It is often associated with some type of strain, either a single injury or a cumulative strain, such as the effects of poor posture. It
is diagnosed with a careful history and physical examination. Myofascial conditions are characterized by tenderness to palpation in discrete areas of the muscle(s), the production of pain into a
remote location with palpation of the tender point, shortening of the muscle length often leading to decreased movement, and focal weakness of the specific muscles(s) due to the shortening, known as
inhibited weakness.
Myofasical conditions are often successfully treated with physical rehabilitation including stretching and strengthening exercises, manual soft tissue techniques, and addressing postural strain issues. The addition of acupuncture or “trigger point injections” are options for more difficult cases.
Osteoporosis - Osteoporosis is defined and diagnosed by a decrease in bone mineral density. Osteoporosis results in decreased mechanical strength and increased likelihood of structural failure. Osteoporosis is the most common skeletal disease associated with aging.
Radiculopathy - Radiculopathy refers to any disease of the
nerve root. Radiculitis indicates actual inflammation around the nerve root; the associated pain is sometimes called radicular pain. Radicular pain may be due to mechanical compression of the nerve
and/or from the chemicals associated with a herniated disc that cause inflammation of the nerve root. See Sciatica.
Sacroiliac Joint Dysfunction - sacroiliac (SI) joint dysfunction is a term to describe mechanical dysfunction of the joint where the ilium and sacrum join. These joints can be seen from the back as two small dimples on each side of the lower back at the belt line, and the ilium has a prominences that can easily be felt just under the skin.
The SI joint is one
of the largest and most stable joints in the body. There are several very strong ligaments that hold the SI joint together. Very little motion occurs in the SI joint and the motion that does
occur is a combination of sliding, tilting and rotation.
SI joint dysfunction
is identified by a detailed physical examination and is controversial as it is not diagnosed with structural tests such as x-rays or MRI scans. Other causes of SI joint pain such as infection, or
inflammation due to conditions like ankylosing spondylitis, are rare, but should be considered. The nerves that go to the SI joints come from many areas of the lumbar spine and sacrum, and
these should be considered as the cause of SI pain as well.
Patients with SIJ dysfunction often have pain over the SI joint that is increased with weight bearing activities such and walking, standing, and running. Pregnancy and unequal leg length may contribute to SI joint dysfunction. Many patients with SI joint dysfunction describe their pain as an “ache” on one side only, however the pain may also extend into the buttock, thigh and leg.
SI joint dysfunction
patients are usually successfully treated with a variety of physical rehabilitation procedures including individualized stretching and strengthening exercises, mobilization and manipulation. Special
belts can be used for patients suspected to have laxity of the ligaments, as in pregnancy. Injections can be employed for difficult cases.
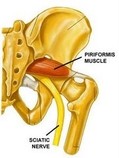
Sciatica - Sciatica is a set of symptoms including pain that may be caused by compression and/or irritation of one of five nerves in the lower back or of the sciatic nerve itself, further away from the spine. The sciatic nerve provides feeling in the buttock, back of the thigh, the lower leg and the foot. When the nerves are pinched, inflamed, or irritated, pain, numbness, and/or weakness can result.
There are different
types of sciatic pain depending on which nerve is irritated:
• Sciatica from L3 nerve root (usually from the L2-L3 level): Symptoms of sciatica coming from this level of the lower back may include: pain and/or numbness to the front of the thigh or weakness of the muscles on the front of the thigh. The patient may also have a reduced knee-jerk reflex. If you have weakness, your knee may feel like it’s going to "give out", and you might notice difficulty getting out of a chair or you might fall.
• Sciatica from L4 nerve root (usually from the L3-L4 level): Symptoms of sciatica coming from this level are very similar to the L3 nerve root and may include: pain and/or numbness to the front of the thigh and inner lower leg and foot; weakness of the muscles on the front of the thigh and/or the inability to bring the ankle upwards. The patient may also have a reduced knee-jerk reflex. If you have weakness, your knee may feel like it’s going to "give out", and you might notice difficulty getting out of a chair or you might fall.
• Sciatica from L5 nerve root (usually the L4-L5 level): Symptoms of sciatica originating at this level may include pain and/or numbness to the top of the foot. The patient may have weakness in lifting the big toe or a foot drop.
• Sciatica from S1 nerve root (the L5-S1 level): Symptoms of sciatica originating at this level may include pain and/or numbness to the outer calf or foot and/or weakness that feels like you can’t push off your toes or walk on the tiptoes. The patient may have reduced ankle reflex.
• Pressure on the sciatic nerve from the piriformis muscle: This pressure on the sciatic nerve is rare as a cause of sciatica but results from tightness of the piriformis muscle deep in the buttock, where it can compress the sciatic nerve. This is called “piriformis syndrome”. Symptoms of piriformis syndrome may include: a sciatica-like pain and/or numbness in the leg, which usually starts in the buttock rather than the low back, often without low back symptoms or signs. Spine movements don’t usually make the symptoms better or worse. Piriformis syndrome can mimic the signs and symptoms of sciatica pain from spinal causes such as a disc herniation and piriformis syndrome should be differentiated from other causes, especially when the diagnosis is unclear.
There are a variety
of conditions that can cause sciatica - these include lumbar disc herniation, lumbar spinal stenosis, piriformis syndrome and others. The cause of sciatica is usually established by a careful history
and examination. It is important to determine if there is evidence of compression or irritation of a spinal nerve root and physical tests of you strength, reflexes and sensation are routinely
performed. Also physical tests that stretch the nerve can be very helpful. X-rays do not show the nerve or the nerve roots, and MRI scans are performed exclusively to confirm the
suspicion of nerve root compression where treatment such as injections or surgery are being considered.
There are a variety
of treatment options for sciatica, depending on the cause.
Scoliosis - Scoliosis is an abnormal side to side curvature of the spine. One or more abnormal curves may be seen when observing the back from behind.
The curvature of the spine from scoliosis may develop as a single curve (shaped like the letter C) or as two curves (shaped like the letter
S).
The two most common types of scoliosis are idiopathic scoliosis (meaning we don’t know exactly what causes it) and degenerative scoliosis:
- Idiopathic scoliosis - the most common form of scoliosis is idiopathic scoliosis, which most often develops in adolescents and typically progresses during the adolescent growth spurt. Because it most often occurs during adolescence, this condition is called adolescent idiopathic scoliosis. This type of scoliosis is much more commonly seen in girls than boys and runs in families. Fortunately, most people will not significantly worsen and interestingly, the vast majority of people with scoliosis are not more likely to have back pain than everyone else.
- Degenerative scoliosis. Scoliosis can also develop later in life, as joints in the spine degenerate and create a bend in the back. This condition is sometimes called adult scoliosis.
Scoliosis has not been linked to the use of backpacks, sports activities, sleeping positions, or posture. Scoliosis is often first noticed by observing that one shoulder or hip is higher than the other. Most people, especially adolescents and children, do not have pain as a result of their scoliosis and it is often observed by a parent, school nurse or pediatrician. The diagnosis of scoliosis is established with a physical examination and the degree of curvature is defined with an x-ray.
Treatment options vary depending on the type and severity, but muscle strength and symmetry can be very beneficial in managing pain. Additional
treatment options, especially for curves that are severe or likely to worsen include bracing and surgery.
Spondylolisthesis - Spondylolisthesis is a condition in which a vertebra has slipped forward in relation to the one below it. This problem can cause both back pain and leg symptoms, however some people have no symptoms with spondylolisthesis.
There are different causes of spondylolisthesis. The two most common causes are:
• Isthmic spondylolisthesis – is typically seen at L5/S1. This typically develops in adolecence and is thought to the result of repeated strain resulting in a stress fracture of a part of the vertebra known as the pars interartcularis.
• Degenerative spondylolisthesis - is most commonly seen at L4/5. Typically develops in middle age or later as a result of degenerative wearing of the cartilage of the facet joints.
Spondylolisthesis is characterized by the percentage of displacement of one vertebra over another. Displacement of over 50% is considered high grade. Spondylolisthesis is diagnosed on an imaging study; x-rays are often initially performed, preferably with the patient standing erect. Additional x-ray views may be obtained with the patient bending all the way forward and backward to determine if there is excess movement of one vertebra on the other. Additional tests such as CT, MRI and bone scans may be also obtained.
The
treatment of spondylolisthesis is usually non-surgical. Exercises to strengthen the back and abdominal muscles are often the primary mode of treatment. Anti-inflammaory medication, steroids or
narcotics can help with the pain and inflammation. Epidural injections can also be effective, primarily for relieving leg symptoms. Surgical treatment becomes necessary when conservative management
fails. Surgery is especially effective for patients with leg symptoms.